The gears of immunity
Not many people know this, but inflammation is the other side of the coin of our immune response. We have also seen this in the pandemic: the most severe cases of Covid-19 are linked to excessive and harmful activation of the immune system.. While for two millennia inflammation has been seen only as something useful, a mechanism that defends us from external attacks, the side effect-often not insignificant-is that this switching on of the immune system over time can contribute to the development of various diseases.. Under scrutiny ischronic latent (or low-grade) inflammation, which is often silent and easily goes unnoticed. Outlining its connections to major noncommunicable diseases are experts at Harvard Medical School. Why is it important to know about this enemy of our health? Because, as the researchers also remind us in their article, targeted actions can be taken to reduce it.
Innate and adaptive immunity
Innate immunity is present from birth and includes granulocytes and the complement system. Granulocytes are short-lived white blood cells that contain small granules that serve to dissolve foreign substances. The complement system, based on about 30 proteins, cascades, participating in the process of defense against infection.
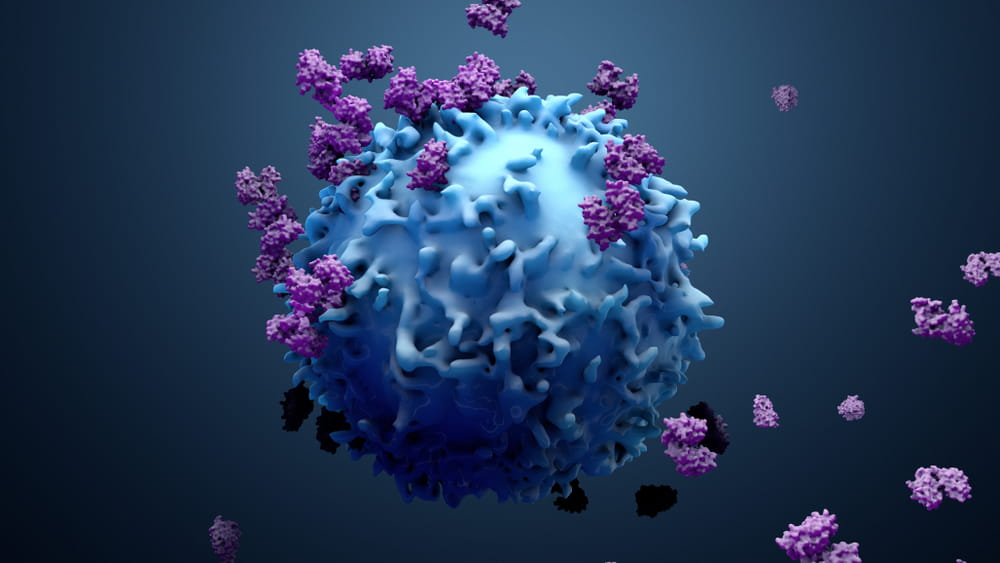
Then there is specific or adaptive immunity, also known as acquired immunity, which is directed in a targeted way against microorganisms we have already encountered, either because of a previous infection or through vaccination, for example.. A central role is played here by T cells-or T lymphocytes-along with B cells and macrophages. T lymphocytesLymphocytes are the cells that make up the effective portion of the adaptive immune system; they are able to generate and modify antibodies that will recognize antigens in the future. They are present in primary lymphoid organs, secondary lymphoid organs, peripheral blood and lymph (where they are currently named). guide the operations by which attempts are made to eliminate microorganisms, directing cells and chemicals to the appropriate place. B lymphocytes produce antibodies directed against the specific pathogen and call up other substances (the complement system) against invasion. Then there are the macrophages–literally big eaters-which act as the “scavengers”of our body, “eating” and eliminating pathogens and other wastes, such as dead granulocytes and waste substances produced in the process of activating the immune system. In this cleansing operation, macrophages acquire information that they pass on to lymphocytes, which in turn will keep a record of it.
According to a Latin saying popular among physicians, inflammation is manifested by “calor, dolor, rubor and tumor,” meaning heat, pain, redness and swelling. The saying, still in use today, refers mainly to acute inflammation, while chronic inflammation is less visible and can be more difficult to detect, both for the patient and the physician
Inflammation and cardiovascular risk
Inflammation and elevated LDL cholesterol levels are two ingredients that can contribute to cardiovascular disease and potentially fatal events such as heart attack. In this case, inflammation can be measured by levels of a marker C-reactive protein (Pcr), in the blood. Those who have elevated levels of C-reactive protein (measured with high-sensitivity tests; read “How to Measure Inflammation” for more details), in fact, would have twice the risk of going on to have a heart attack, twice the risk of going on to have a heart attack, and the likelihood is even greater if LDL cholesterol is also high.. The reason? When LDL cholesterol becomes oxidized, it is easily recognized and ingested by macrophages: loaded with lipids, these immune system cells are deposited on the artery wall and covered with fibrous tissue, forming atherosclerotic plaques. In some cases, when they grow and when their lining is under stress, these plaques can rupture and clots can clog a coronary artery, causing a heart attack.

Macrophages are the scavengers of the immune system: they phagocytize and eliminate pathogens, infected cells, and cellular debris. They also contribute to the mechanisms of immunological memory
Inflammation and diabetes
Some large observational studies (in which researchers do not directly intervene but merely observe a certain phenomenon) have shown an association between high Pcr levels and insulinHormone produced by Langerhans island cells of the pancreas. It stimulates the entry of glucose into the cells, subtracting it from the blood and thus lowering blood sugar. It induces the use of glucose both to produce energy and for the synthesis of glycogen and fats. resistance. Insulin resistance, which is often the prelude to diabetes, occurs when cells do not allow insulin to enter them, resulting in blood glucose not being metabolized adequately.
Inflammation and cancer
There is also a close link between inflammation and cancer. Almost 150 years ago, pathologist Rudolf Virchow noticed that tumor tissue contains high concentrations of inflammatory cells and hypothesized that tumors formed at sites where there is chronic inflammation. His hypothesis was later confirmed: about 15 percent of malignant tumors are stringently linked to certain infections.. Certain substances produced in an inflammatory reaction, such as free radicalsA free radical is a particularly reactive molecule or atom that contains at least one odd electron in its outermost orbital. Because of this chemical characteristic, free radicals are highly unstable and try to return to equilibrium by stealing from the nearby atom the electron needed to equalize its electromagnetic charge. This mechanism gives rise to new unstable molecules, triggering a chain reaction that, if not stopped in time, ends up damaging cellular structures and metabolic processes., can damage the DNA of cells and promote the development of cancer cells. Again macrophages come into play: these molecules, which have the role of eliminating microorganisms and waste products, can produce tumor growth factors and promote the proliferation of blood vessels that feed cancer cells.
Some substances produced in an inflammatory reaction, such as free radicals, can damage the DNA of cells and promote the development of cancer cells
Inflammation and Alzheimer’s
The blood-brain barrier defends the brain from potentially dangerous external attacks, such as infection, and inflammation. While we are quite protected from the outside, some damage can occur within this barrier. Here microglia cells, the brain counterpart of macrophages, scurry and engulf foreign substances releasing inflammatory molecules.. When this release is excessive, problems can occur: this is the case with beta-amyloid protein, which is thought to play a major role in Alzheimer’s.. Microglia cells incorporate beta-amyloid, forming the plaques characteristic of the disease.
We delved into the methods most widely used today to measure chronic latent inflammation in another article you will find on the SoLongevity website.